The plant has been used for therapeutic purposes for millennia. Prohibition hindered research and knowledge remains limited, but positive effects have been demonstrated in several diseases.
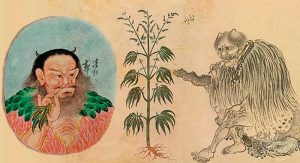
The Cannabis sativa plant has been known to humankind for a very long time. The oldest known written document detailing some of the medicinal properties of cannabis dates back to 2727 BC. In this text, the Chinese emperor Shen-Nung enthusiastically proclaimed the therapeutic benefits of cannabis as if it were an ancient miraculous balm. He recommended the medicinal use of cannabis for more than 100 different diseases (ranging from constipation to gout, including malaria and rheumatism).
Over the course of thousands of years, this plant spread from the Far East to the rest of the world. Today, cannabis (better known as marijuana) is the most widely used illegal psychoactive drug in the world, primarily for recreational purposes and, to a much lesser extent, for therapeutic purposes.
In a survey conducted in our country, one in three Spaniards acknowledged having tried marijuana at least once in their lifetime. According to another survey by the Ministry of Health, 7.6% of Spaniards reported having consumed marijuana in the past month. In addition, the Spanish Observatory of Medicinal Cannabis (OECM) estimated that between 50,000 and 100,000 consumers use it for therapeutic purposes.
Cannabis is a very complex plant, as it contains more than 500 different chemical compounds. More than 150 of them are cannabinoid compounds that have specific effects on the human brain by acting on certain receptors (also called cannabinoid receptors). The two main molecules responsible for the typical effects of cannabis are tetrahydrocannabinol (THC) and, to a lesser extent, cannabidiol (CBD).
These molecules are found in their acidic form in the plant and, under these conditions, do not produce effects on the human body. It is necessary to heat these compounds beforehand so that their chemical structure changes slightly and they can then act on the human brain.
On the other hand, both THC and CBD are highly fat-soluble and dissolve very poorly in water. This chemical property means that, in addition to having a special affinity for the brain (which has a high fat content), they also migrate to the body’s fatty tissue.
Thus, around 10% of these cannabinoids go to the brain and 90% to adipose tissue, where they also accumulate. It is precisely this accumulation in fatty tissue that causes THC and CBD to remain present in the body for days or even weeks after occasional cannabis use. Therefore, unlike many other drugs, the half-life of these cannabinoids in the human body is considerably longer.
The characteristic psychoactive effects of marijuana are mainly due to the changes it produces in the neurons of the endocannabinoid system. This system is involved in the regulation of a wide range of functions (memory, appetite, pain, sleep, body temperature, stress response, etc.).
Molecules such as THC and CBD act as if they were cannabinoid neurotransmitters naturally present in our brains (anandamide and 2-AG), due to similarities in their molecular structures. Thus, both THC and CBD bind to the receptors to which our own neurotransmitters normally bind, replacing their function and producing various effects. Even so, the main effect of CBD is mediated by an increase in 2-AG, since its affinity for cannabinoid receptors is low and it is not considered a psychoactive molecule.
In addition to the actions of these molecules on the endocannabinoid system, indirect stimulation of the brain’s reward system (which provides pleasure and well-being) also occurs. Dopamine release is increased by blocking the release of a neurotransmitter (GABA) that inhibits dopamine release. It is this stimulation of the reward system, together with binding to cannabinoid receptors (mainly due to the action of THC), that produces the typical “high,” in which euphoria and well-being are experienced.
Barriers to research
Despite the fact that humans have cultivated and consumed cannabis for thousands of years, scientific research into its psychoactive molecules and pharmacological properties began very late, specifically at the end of the 19th century. Furthermore, the widespread illegalization of cannabis in many parts of the world in the 1930s was—and continues to be—a major obstacle to scientific research.
Researchers in this field have faced and continue to face numerous administrative, financial, legal, and political obstacles stemming from the illegal status of cannabis. As a result, knowledge about the therapeutic effects of cannabis is very limited compared to other drugs, due to the barriers imposed for nearly a century. In fact, the endocannabinoid system present in humans was discovered less than 35 years ago. Thus, many details about cannabis and its effects on human health remain unknown today.